Activated T cell therapy developed for advanced melanoma
Source: Oncology Nurse Advisor, July 2015
Source:OncologyNurseAdvisor
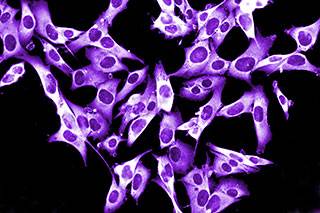
T cells from patients with melanoma can trigger a protective immune response against the disease according to data from an in vitro and animal study. The findings were published in the Journal of Immunotherapy (2015; doi:10.1097/CJI.0000000000000078).
The new findings demonstrate that T cells derived from lymph nodes of patients with melanoma can be expanded in number and activated in the laboratory for intravenous administration in the treatment of patients.
The research team was led by Julian Kim, MD, Chief Medical Officer at University Hospitals Case Medical Center Seidman Cancer Center and at Case Western Reserve University School of Medicine in Cleveland, Ohio.
They developed a novel technique to generate large numbers of activated T cells that can be transferred back into the same patient to stimulate the immune system to attack the cancer.
“This study is unique in that the source of T cells for therapy is derived from the lymph node, which is the natural site of the immune response against pathogens as well as cancer," said Kim. “These encouraging results provide the rationale to start testing the transfer of activated T cells in a human clinical trial."
Kim and his team developed a new method to grow and activate immune cells in a two-week culture. Immune cells are extracted from lymph nodes that have been exposed to growing melanoma in the patient’s body.
Rather than trying to activate the T cells while in the body, the lymph nodes are surgically removed so that the activation process and growth of the T cells can be tightly regulated in a laboratory.
This novel approach to cancer treatment, termed adoptive immunotherapy, is only offered at a few institutions worldwide.
These promising findings have led to the recent launch of a new phase 1 human clinical trial at UH Seidman Cancer Center in patients with advanced melanoma.
RELATED: Mechanism discovered for BRAF inhibitor resistance in melanoma
The research leading to the clinical trial was funded by the National Institutes of Health and the Case Comprehensive Cancer Center.
The trial is being supported by University Hospitals as well as a significant philanthropic effort including the Immunogene Therapy Fund, the Paula and Ronald Raymond Fund, and the Kathryn and Paula Miller Family Fund.
“The infusion of activated T cells has demonstrated promising results and is an area of great potential for the treatment of patients with cancer," said Kim.
“We are really excited that our method of activating and expanding T cells is practical and may be ideal for widespread use. Our goal is to eventually combine these T cells with other immune therapies which will result in cures."
Additionally, the team has been researching the possibility of using lymph nodes from patients with pancreatic cancer to develop T cell therapy. Their goal is to expand the program and eventually study other tumor types including lung, colorectal, and breast cancers.
