Navigating the Changing Melanoma Landscape
Source: Clinical Oncology, July 2014, by Kate O’Rourke
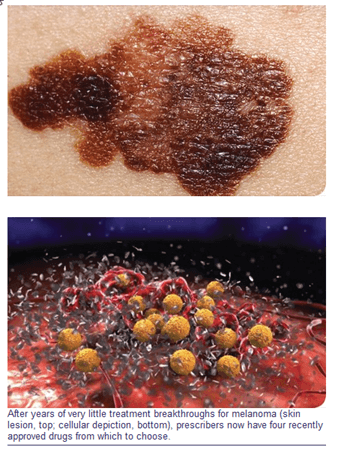
Since 2011, four new medications have arrived on the scene for treating patients with melanoma. That’s good news for a potentially deadly cancer that had not seen a new drug approval in the preceding decade. Still, the glut of new treatment options does pose some significant management challenges.
Vananh Trinh, PharmD, BCOP, a clinical pharmacy specialist at the University of Texas MD Anderson Cancer Center, in Houston, said that sequencing the available agents could be a particularly thorny issue. When patients with melanoma first present, Dr. Trinh noted, should they be started on high-dose interleukin-2 (IL-2), one of the mainstays of therapy? Or should one of the newly approved agents—ipilimumab (Yervoy, Bristol-Myers Squibb), vemurafenib (Zelboraf, Genentech), dabrafenib (Tafinlar, GlaxoSmithKline) or trametinib (Mekinist, GlaxoSmithKline)—be the first choice?
These can be tough decisions. Fortunately, patient selection criteria (e.g., mutation type and tolerance to side effects) and clinical trial data often will point clinicians in the right direction, Dr. Trinh said during a melanoma update session at the recent annual conference of the Hematology/Oncology Pharmacy Association.
The Drugs and Their Class
Ipilimumab is a monoclonal antibody that blocks cytotoxic T lymphocyte–associated antigen 4 to enhance an antitumor T-cell response. In a clinical trial, patients who received the drug had a better median overall survival (OS) than patients receiving a glycoprotein 100 peptide vaccine (10.1 vs. 6.4 months; hazard ratio [HR], 0.66; P=0.003; N Engl J Med 2010;363:711-723). This is an achievement, considering that the older standard-of-care regimens such as dacarbazine, temozolomide, high-dose IL-2, combination chemotherapy and biochemotherapy have never been proven to improve OS in randomized Phase III trials, Dr. Trinh said.
Vemurafenib and dabrafenib are BRAF kinase inhibitors and should only be used in patients with BRAF mutations, he pointed out. The two drugs inhibit mutant BRAF kinase, which plays a role in the regulation of cell growth. Approximately 50% of patients with melanoma have these mutations.
In the BRIM-3 (A Study of RO5185426 in Comparison With Dacarbazine in Previously Untreated Patients With Metastatic Melanoma) updated analysis, vemurafenib showed a substantial improvement over dacarbazine with a median OS of 13.2 months versus 9.6 months (HR, 0.37; P<0.001; Lancet Oncol 2014;15:323-332). The BREAK-3 study pitted dabrafenib against dacarbazine (Lancet 2012;380:358-365). The median progression-free survival (PFS) was roughly double in patients receiving dabrafenib (5.1 vs. 2.7 months; HR, 0.30; P<0.0001). Comparing the two BRAF inhibitors, Dr. Trinh pointed out that in BRIM-3, patients receiving vemurafenib had a median PFS of 5.3 months (N Engl J Med 2011;364:2507-2516). The downside of BRAF inhibitors, she said, is that many of the responses are partial responses and the duration of response is often short.
Trametinib is a mitogen-activated extracellular signal-regulated kinase (MEK) inhibitor. In a Phase III trial, patients given trametinib had a median PFS of 4.8 months compared with 1.5 months in patients receiving chemotherapy (HR, 0.45; P<0.001; N Engl J Med 2012;367:107-114). The hazard ratio for death was 0.54 (P=0.01). In an updated analysis presented at the 2013 meeting of the Society for Melanoma Research, in Philadelphia, the median OS in the trametinib-treated group was roughly 15 months(Pigment Cell Melanoma Res 2013;26:997).
Dr. Trinh explained that BRAF inhibitors cause paradoxical mitogen-activated protein kinase (MAPK) activation in some tissues and should not be used in patients with mutant NRAS or wild-type BRAF melanoma. “This paradoxical activation of the pathway can also explain a unique side effect of BRAF inhibitors, which is patients can develop cutaneous squamoproliferative lesions and other secondary malignancies,” she said. “MEK inhibitors, on the other hand, have no issue with paradoxical MAPK activation.”
Immunotherapy First!
Anthony Jarkowski, PharmD, BCOP, a clinical pharmacy specialist at the University of Rochester Medical Center, in Rochester, N.Y., who also spoke during the HOPA session, argued that immunotherapy should be used first in patients and BRAF inhibitors should be the second in the sequence, as long as patients actually have a BRAF mutation. He maintained that BRAF inhibitors have a short duration of response and only between 1% and 3% of patients have a complete response. “I am a huge believer in immuno-oncology. I think that is where the future is headed,” he said. “A lot of the responses that we see with the BRAF inhibitors are partial responses.”
Dr. Jarkowski pointed out that at around five to six months, patients start to progress on BRAF inhibitors. “The big thing that you have to remember is that about 40% to 50% of patients that progress on BRAF inhibitors die within 28 days of their last dose of the BRAF inhibitor. So, you have a 50/50 shot of making it to another therapy.”
High-dose IL-2 therapy, he said, has shown greater evidence of producing durable complete responses in the patients who actually respond to the drug, albeit that response rate is fairly low (16%) in a pooled analysis of 270 patients from eight clinical trials (J Clin Oncol 1999;17:2105-2116).
Dr. Jarkowski noted that updated data from the previously mentioned ipilimumab trial have shown that this immunotherapy can have long-lasting effects. Survival rates at two and three years were 25% in patients who received ipilimumab (Ann Oncol 2013;24:2694-2698).
In another study, a pooled analysis of three trials, all but one of 15 patients who had a complete response to ipilimumab was still alive at 54 to 99-plus months (Clin Cancer Res 2012;18:2039-2047). This same study showed that it took an average of 30 months for patients to achieve a complete response. “What you have to remember about immunotherapy is that [it] takes a lot of time to work,” Dr. Jarkowski said.
BRAF Inhibitors
LeAnn Norris, PharmD, BCOP, an assistant professor of pharmacy at the South Carolina College of Pharmacy, Charleston, argued during the HOPA session that BRAF inhibitors should be the agent of first choice for patients with melanoma who have a BRAF mutation. She pointed out that the response and survival rates are better with BRAF inhibitors (Table). Additionally, compared with ipilimumab, BRAF inhibitors are much more tolerable, with fewer adverse drug events and a faster median onset of response (vemurafenib, 1.45 months; dabrafenib, 6.3 weeks) (N Engl J Med 2011;364:2507-2516; N Engl J Med 2010;363:711-723). “If you have a patient who is very sick, perhaps with multiple comorbidities, multiple metastases, etc., and you really want to initiate therapy where they can hopefully get a very quick response, then the [BRAF inhibitors] are the appropriate treatment options,” Dr. Norris said.
|
|||||||||||||||||||||||||||||||||||
When Dr. Norris looks at a patient, she considers whether that individual is going to be able to handle the burdensome side effects of immunotherapy, which include skin/mucosal problems, diarrhea, colitis and hepatoxicity. She pointed out that 60% of patients experience an adverse drug event with a mean time to resolution of 6.3 weeks (N Engl J Med 2011;364:2507-2516). “Sequencing doesn’t really mean anything if we can’t get a patient through the immunotherapy first,” Dr. Norris said. “For a lot of our patients who present with very bad disease, a poor prognosis, multiple metastases and comorbidities, BRAF inhibitors are probably going to be the first ones you reach for.”
She pointed out that MEK inhibitors have low toxicities as well, but a response rate of roughly 22% and a short duration of response (N Engl J Med 2012;367:107-114).
Dr. Trinh said the two arguments favoring first-line therapy that were presented during the HOPA session were very convincing. “Only a randomized controlled trial that directly compares the different sequences will actually break the tie,” she said, “[so] at this time we can only individualize patient therapy.”
