Math formula helps predict melanoma treatment success
Source: The SunCoast News, December 2014
An anti-cancer medicine the Food and Drug Administration approved for clinical use in September has shown encouraging success in treating people with advanced cases of the deadly skin cancer melanoma.
Unfortunately, the drug, pembrolizumab, only works that well in 30 percent of melanoma sufferers.
Researchers at the UCLA Jonsson Comprehensive Cancer Center have been working on a method to determine which people with melanoma are likely to benefit from pembrolizumab, which is marketed by Merck under the brand name Keytruda.
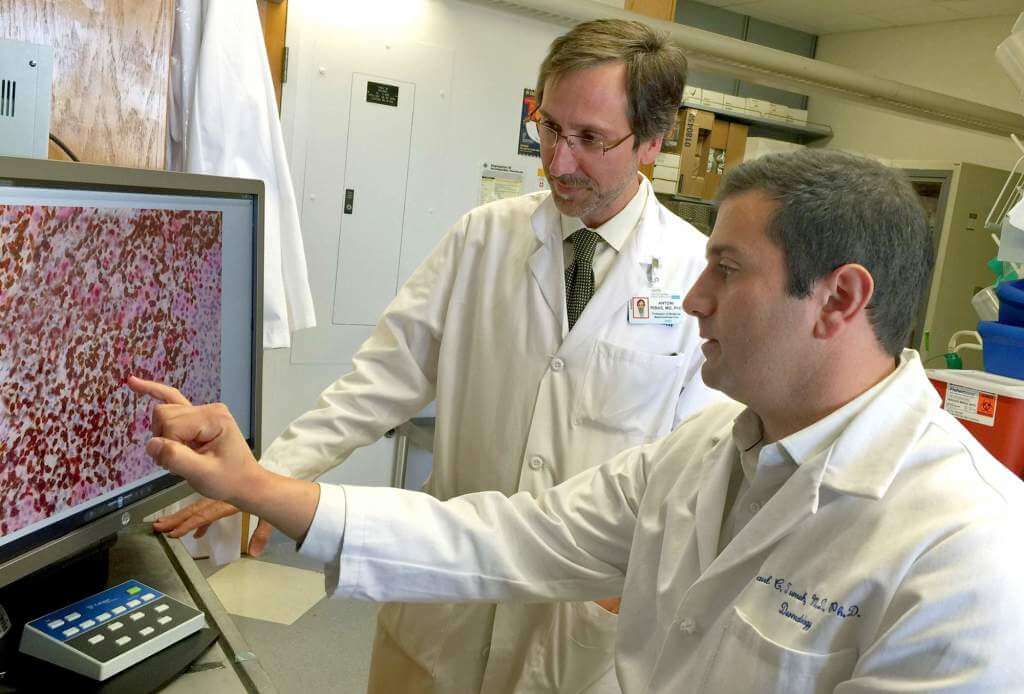
“We’ve had amazing clinical success treating patients battling advanced melanoma with pembrolizumab. The challenge is that it only works in approximately 30 percent of patients with melanoma,” said Paul Tumeh, lead author of the UCLA study and assistant professor of dermatology. “To address this challenge, we developed an approach that can select for patients that are likely to respond to this therapeutic class.”
Tumeh’s co-leader in the study is Antoni Ribas, professor of hematology and oncology.
Pembrolizumab, a mo- noclonal antibody drug, works by keeping a protein molecule known as PD-1 from blocking the immune system component known as T cells, say scientists. With PD-1 disabled, the white blood cells should attack and destroy cancerous cells in melanoma patients.
Tumeh and Ribas have spent two years studying 46 melanoma patients who had been treated with pembrolizumab. The study subjects underwent tissue biopsies before and during the anti-cancer immunotherapy treatments.
They analyzed the biopsy samples and classified them according to whether the patient responded to pembrolizumab. With that data in hand, Tumeh and Ribas, with the help of UCLA adjunct professor of medicine David Elashoff, developed an algorithim they believed could predict which melanoma patients are likely to have success with pembrolizumab.
To test the mathematical formula, they applied it to tissue samples from 15 melanoma patients in Paris who had received pembrolizumab. The UCLA researchers did not know how the French patients had responded to the treatments.
The algorithim correctly determined how 13 out of the 15 the patients did on pembrolizumab.
Pembrolizumab was the first PD-1 immunotherapy drug to receive FDA approval, but three others are undergoing clinical development. Tumeh and Ribas believe their findings, published Nov. 26 via the online version of the journal Nature, will help researchers and physicians create additional drugs for use against melanoma and perhaps other types of cancer.
“The next big step is to classify the different types of patients that do not respond to treatments so we could modulate the drug to target their tumors,” said Tumeh.
This research was supported by Stand Up to Cancer and the National Institutes of Health. Additional funding was provided by the UCLA Jonsson Comprehensive Cancer Center through philanthropy and other sources.
